Registries are very helpful. They can help with identifying and directing patients towards programs and projects. They can help with industry sponsored studies. Registries can be used to better understand a clinical problem and help answer many questions especially when supported by large numbers of participants. Registries can also help with awareness of a problem. It is easy to see how it can be a voice for those affected by a condition. It is also a way of organizing and standardizing a problem.
FARE has a patient registry. It is for those affected by and for those who take care of individuals with food allergy.
I signed on yesterday- even a watermelon allergy would qualify for the registry.
FEL 11/14/2017

https://www.foodallergypatientregistry.org
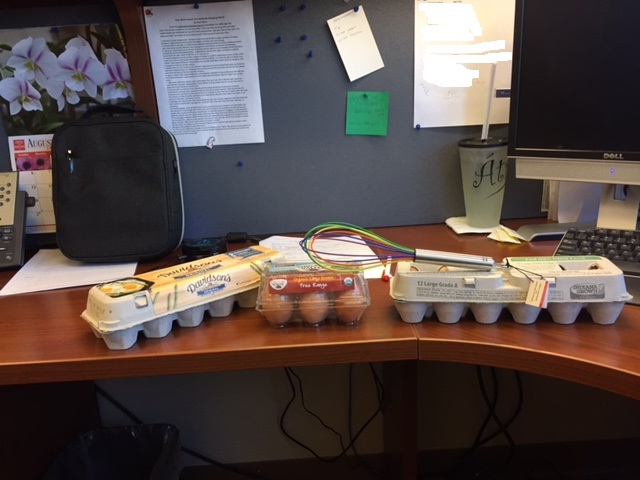
A college student came in for an egg challenge today. He forgot to bring the challenge food with him.
Our site is across the street from a grocery store. He was told to go there and return with ‘Egg Beaters’ (the product we use to do egg challenges with).
Pictured below is what he came back with-
I write this entry with a tear in my eye. In the Sunday Indianapolis Star I read the following story ‘Alas, the Pontiac- R.I.P..

Mr. Dan McFeely noted on the next line that ‘Aficionados lament General Motors’ decision to end production of the brand now likely to be a hot classic’. The obituary noted that GM life support for Pontiac was pulled on April 27th, 2009. Pontiac (nee the Oakland Motor Car Company) was born in 1926 in (appropriately) Pontiac, Michigan. Pontiac was the proud parent of GTO, Firebird, Catalina, Grand Prix, Bonneville, the Chief, the Star Chief, Fiero, and my beloved Lemans (just to name a few ).
I owned a 1967 Pontiac Lemans convertible in 1973. I had that car for six months before it became car number five in a six car sandwich. The car was totaled in April in Cleveland, Ohio. I never had a chance to put the top down and enjoy it. I owned it for six months of which only one month was considered spring (I lived in Cleveland at the time).
In 2001 I thought I had seen a ghost. Appearing on the internet was the exact same car. It was the same color, the same year, the same make, the same everything. It was for sale in Southern California by its second owner who enjoyed driving the car to the beach with his surf board in the back.
Friends of mine looked at the car and I made the purchase. For the past eight years I have an exact copy of my 1967 Lemans (as I remember it from 1973).
I am sure you have all heard of the GTO and perhaps not so much about the Lemans. The Lemans has been called the poor man’s GTO. It has a very similar shape and look. This is my toy.

1967 Pontiac Lemans and home.

1967 Lemans – top down and ready to go cruising for burgers.

No 1967 muscle car would be complete without a hula girl on the console. This was courtesy of ‘Old Blue’s’ previous owner.
Fred Leickly
I receive the journal Contemporary Pediatrics. I have found the articles to be very practical for everyday use. For the most part the authors are reviewing a specific topic of interest. An author will condense a large volume of literature into a very readable format. Back in the day, I was asked to write an article about chronic hives for Contemporary Pediatrics. I titled that article ‘When the road gets bumpy, chronic urticaria’. I enjoy reading Contemporary Pediatrics and I have used interesting findings in this blog (see my note on the ‘Patient History’)
I always scan the articles and a while back I came across a little quip that caught my attention. It made me wonder about the many times I had suggested using a teaspoon measure of medication.
When we prescribe medications we all have the tendency to use the teaspoon/tablespoon measure of delivery. Our assumption is that a teaspoon is five milliliters (mls) and a tablespoon is three teaspoons so that would equate to 15 mls. The question was asked whether or not teaspoons are standardized. I discovered that they clearly are not and the use of teaspoons for dosing could lead to more overdosing as opposed to under dosing.
So the question is, do you use mls or teaspoons?
The article was amazing- It was a clinical tip about the timely death of the ‘teaspoon’ at least for giving medications. The work was done by Alvin N. Eden, MD, and Mohammad Mir, MD Department of Pediatrics, Wyckoff Medical Center Brooklyn, N.Y. and appeared in the November 1, 2008 Contemporary Pediatrics.
The background is that more than 50% of liquid preparations given to children are written as a number of teaspoons. This small research project looked at the volume of 53 teaspoons brought in by physicians, nurses, and the receptionists at a general pediatric practice. Only one of the teaspoons actually measured 5 milliliters. The range was 4.3-12.9 mls! Based on these findings, using the tsp format could result in overdosing by 2.5 times the intended dose.
This made me think about the use of oral steroids for our children who have a flare of their asthma. The medications are 15 mg per 5 mls and the dose would be 2 mg/kg of body weight per day. If a teaspoon that measured 12.9 mls was used, then 38.7 mg were given and not the intended 15 mg! Steroid side-effects could occur due to the over-exposure via generous teaspoons.
Due to this extreme variability in volume and the chance of an overdose, the milliliter format was suggested as the proper way to administer liquid medications.
Go metric- ask for how many milliliters and use the proper dosing apparatus.
Fred Leickly
Physicians Practiceis one of those many journals that finds itself on my desk. I usually browse through the articles while enjoying a quick lunch. I am on the subscriber list due to my connection with the Indiana University Medical Group. The journal deals mostly with practice management which is great for someone in private practice. In February of this year Physicians Practice did published a case report that I wrote. The case involved the critical role allergy has in asthma diagnosis and management. For the most part this journal has articles about electronic medical records, coding, dealing with health insurance companies and so on. Many of these topics are interesting, but do not have a direct impact for someone working in an academic center. However, the April edition of Physicians Practice has a very interesting article (page 26) on ‘Evidence-Based Medicine’. The attention getting statement certainly made me take a look, “Evidence-based medicine has been around for 16 years. So why are some physicians still resistant to it? And how can you make it work for you?”
Evidence-based medicine (EBM) tries to provide a framework for treatment that is supported by the latest proven research. The article talks about this enhancing a medical practice. I think that patients and families should be aware of EBM. I can see value of EBM in the practice of allergy by board-certified allergists especially in an environment where the label of ‘allergy’ is given too loosely. In my practice I am seeing conditions labeled as allergy (apraxia, autism, sensory integration defects, ADHD to name a few) because tests for allergy return as positive. Many times the clinical condition and the test has nothing to do with allergy. IgG to food would be a prime example. I have seen significant amounts of money spent and hopes of families dashed by the use of tests and therapies that are not evidence-based.
The EBM approach first asks a very specific clinical question. The question could be about a test, a treatment, a diagnosis, or an outcome. Next the literature is searched for information on the topic. The information is then evaluated to see if it is valid, useful, and related to the question. The review of the literature looks critically at many different aspects of the scientific studies. The numbers, the methods, and the statistics are evaluated. The EBM may conclude that there exists type A evidence (great supportive studies in a large number of patients) that a treatment is effective.
Other support for diagnosing and treating can be found in ‘Guidelines’ . Many specialty organizations offer guidelines for common clinical conditions and the guidelines will incorporate EBM.
Resistance to EBM stems from concerns that it is a cookbook approach to medical practice. Another issue is how can a busy practitioner integrate EBM into a practice. The article provides ideas and links for the practitioner.
Now the journal also had an excerpt from an article written by D. Isaacs and D. Fitzgerald that appeared in the British Medical Journal a few years ago (BMJ 1999;319:1618) that poked a little fun at EBM. What follows was the results of a poll that asked physicians what they would do if there was no solid evidence in the literature to help with a clinical decision. The article was titled, “Seven alternatives to evidence-based medicine”. This made me smile.
- Eminence Based Medicine- The more senior the person, the less need for evidence. Experience outweighs evidence. Faith in clinical experience was defined as making the same mistake with increasing confidence over an impressive number of years.
- Vehemence Based Medicine- Substituting volume for evidence as an effective technique for brow-beating a more timid colleague.
- Eloquence Based Medicine- The perennial sun tan, carnation on the Armani suit, the silk tie accompany a tongue as equally smooth. Tailored eloquence and verbal eloquence are powerful substitutes for evidence.
- Providence Based Medicine- If the caring practitioner has no clue what to do next, the decision may be best left in the hands of the Almighty.
- Nervousness Based Medicine- The fear of litigation is a driving force for more tests and excessive treatments.
- Confidence Based Medicine- Restricted to surgeons
Now I am puzzled- the quip in Physicians Practice said seven, I count only six. This second article ended and I could not find that seventh alternative. Finally, I found the original article at the Ruth Lilly Library on OVID. Here is number seven.
- Diffidence Based Medicine- Some doctors see a problem and look for an answer. Others merely see a problem. The diffident doctormay do nothing from a sense of despair. This, of course, may bebetter than doing something merely because it hurts the doctor’spride to do nothing (BMJ, 1999).
That was the original article on alternatives to EBM. Now it gets even better. Others have added to this list, we now have the following alternatives; Effervescence Based Medicine, Webidence Based Medicine, Profit Based Medicine, Annoyance Based Medicine, Propaganda Based Medicine, and Arrogance Based Medicine to name a few. We see a significant amount of Webidence Based Medicine. I urge caution with the internet. Look to sites sanctioned by well known organization- the American Academy of Pediatrics, the American Academy of Allergy, Asthma, and Immunology, the Food Allergy and Anaphylaxis Network, the National Institutes of Health, the National Heart, Lung, and Blood Institute to name a few. Profit Based Medicine – as a personal word of caution, ask about insurance coverage. Your insurance may not cover something because it is experimental or without EBM to support what is done. There is usually a reason why something is not covered by insurance. Ask about it.
I do my best to abide by evidence- based medicine. It makes sense to me. Evidence for my diagnosis, evidence for my selection of tests to help with that diagnosis, and evidence for the best treatment for the condition. Medicine is changing all the time. EBM helps evaluate what we have done and helps to consider what we need to do for the benefit of those we are taking care of.
Fred Leickly
This is my granddaughter Stella. Stella is about to celebrate her first birthday this week. Her dad took this picture (I found it on his flickr site) and it is precious. It made me think of how avoidance of foods by those allergic to them may be somewhat difficult especially for curious and mobile toddlers.
Cheerfully submitted,
Fred Leickly
